Your grandmother keeps telling you that her knee osteoarthritis hurts more when it's cold, and your brother-in-law complains about his rheumatoid arthritis on rainy days. Your neighbor even claims he can predict tomorrow's weather based on his hip pain.
The idea that the weather influences rheumatism is very common. In fact, a quick search on any search engine will confirm this. [1] Discussions on medical forums and blog pages abound in an attempt to answer this curiosity about the human body: is there really a link between the weather and our rheumatic pain?
Cold and rain often blamed
The onset of winter is not always very pleasant, as people with persistent pain know only too well. In fact, 80% of people with persistent pain cite the weather as the second most important factor in maintaining their pain. Variables such as cold and rain are the most commonly cited, but other variables have also been analyzed in recent studies, such as atmospheric pressure, humidity, sunshine, cloud cover, and wind gusts.
However, these studies have produced conflicting results (as is often the case in health sciences). While some highlight a link between low temperatures and pain, others come to the opposite conclusion. And the situation is repeated with other variables such as humidity, gusts of wind and atmospheric pressure. In addition, all of these studies had methodological limitations: the groups of people were not large or diverse enough, weather conditions and symptoms were monitored over too short a period, there were no records of weather conditions where people live and work, and there were other biases that could have affected pain levels, such as sleep, mood, and physical activity. [2, 3]
A smartphone app as the solution?
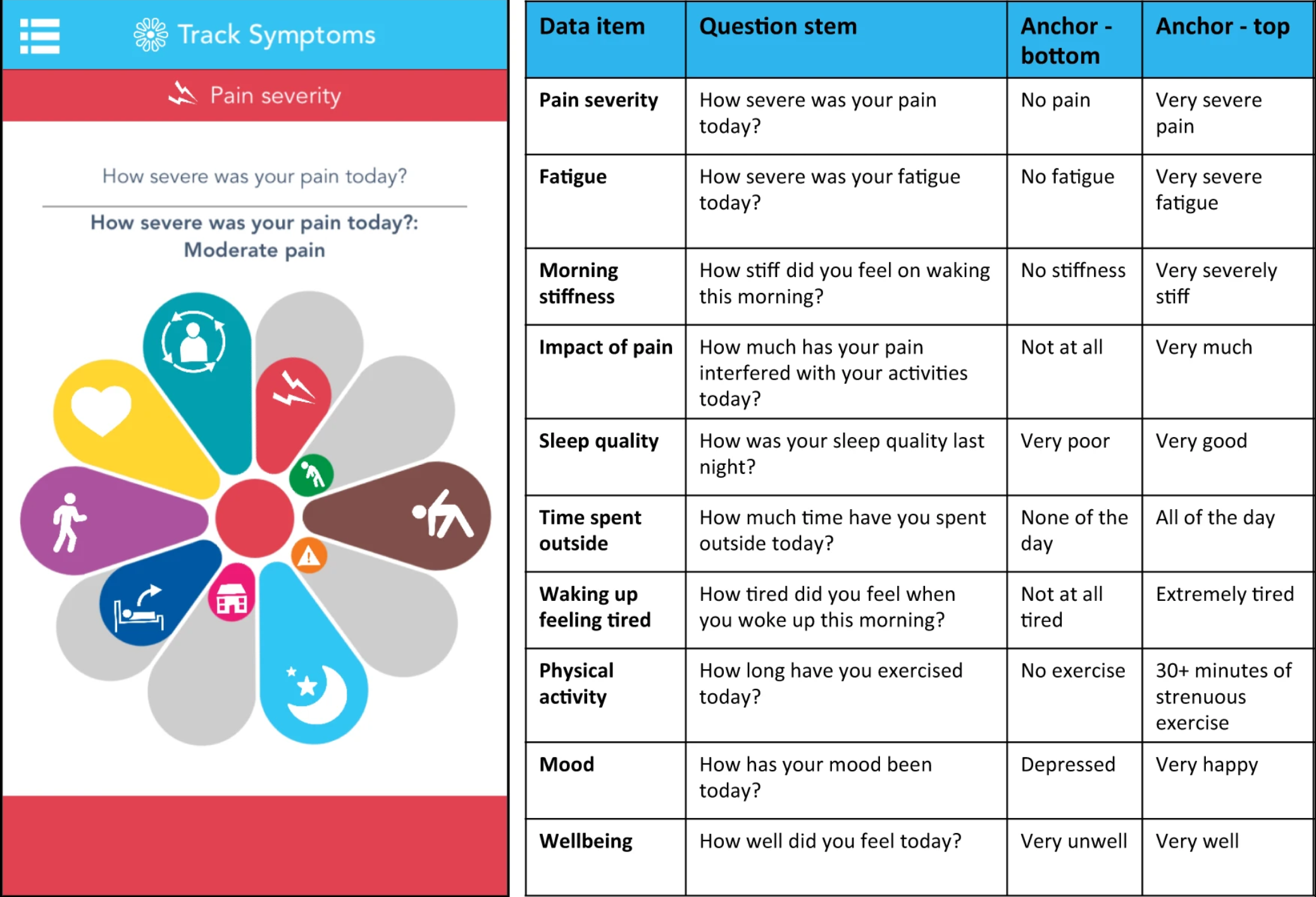
In an attempt to eliminate these biases and understand which weather conditions most affect pain, a group of researchers from the University of Manchester conducted a year-long study of 13,000 British residents living with chronic pain between 2016 and 2017. [4] Participants recorded the intensity of their pain each day in a smartphone app (“cloudy with a chance of pain”) (see image). Weather data was determined based on the GPS location of their phones. The researchers then compared the pain reported on days with good weather and days with bad weather. The analysis consisted of disentangling the relative importance of different weather components (specifically, temperature, humidity, wind, and pressure).
Results that confirm beliefs
This study identified several interesting points. These points are consistent with the beliefs of many patients.
First, an increase in pain is observed under certain weather conditions. In order of importance: higher humidity, lower pressure, and stronger winds.
In short, bad luck for the Bretons... However, no association was found with temperature. So, for example, dry, cold weather with no wind would not be associated with increased pain.
Secondly, the weather most likely to be associated with increased pain was a humid, windy day with low pressure.
Thirdly, the weather least likely to be associated with increased pain was a dry, calm day with high pressure.
Finally, on a day with “bad weather” (humid, low pressure, windy), people were 20% more likely to experience pain than on a day with average weather.
A better understanding of the effects of the environment on pain could enable scientists to better understand the mechanisms behind pain and develop new, more effective treatments for people who suffer from it.
But in the meantime, there's no question of staying on the couch on bad weather days. Keeping active, whatever the activity and how long you do it for, remains a key ally in the fight against persistent pain.
Sources :
[1] Telfer, Scott, and Nick Obradovich. “Local Weather Is Associated with Rates of Online Searches for Musculoskeletal Pain Symptoms.” PLoS ONE, vol. 12, no. 8, Aug. 2017, p. e0181266, doi:10.1371/journal.pone.0181266.
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0181266
[2] Beukenhorst, Anna L., et al. “Are Weather Conditions Associated with Chronic Musculoskeletal Pain? Review of Results and Methodologies.” Pain, vol. 161, no. 4, Apr. 2020, pp. 668–83, doi:10.1097/j.pain.0000000000001776.
https://journals.lww.com/pain/Fulltext/2020/04000/Are_weather_conditions_associated_with_chronic.3.aspx
[3] Duong, Vicky, et al. “Does Weather Affect Daily Pain Intensity Levels in Patients with Acute Low Back Pain? A Prospective Cohort Study.” Rheumatology International, vol. 36, no. 5, May 2016, pp. 679–84, doi:10.1007/s00296-015-3419-6.
https://link.springer.com/article/10.1007%2Fs00296-015-3419-6
[4] Dixon, William G., et al. “How the Weather Affects the Pain of Citizen Scientists Using a Smartphone App.” Npj Digital Medicine, vol. 2, no. 1, Oct. 2019, pp. 1–9, doi:10.1038/s41746-019-0180-3.